Contents
Non-Invasive Prenatal Test (NIPT)
What is Non-Invasive Prenatal Testing?
Who does the NIPT screening?
What is the cost of the NIPT screening test?
Who has NIPT screening?
So I still need a 12-week ultrasound scan?
Are there problems the NIPT test will not detect?
What are the limitations of the NIPT Test?
Related articles
 This is a new non-invasive way of checking your baby’s chromosomes and so excluding the most common chromosome disorders with a very degree of accuracy, the Non-Invasive Prenatal Test (NIPT).
This is a new non-invasive way of checking your baby’s chromosomes and so excluding the most common chromosome disorders with a very degree of accuracy, the Non-Invasive Prenatal Test (NIPT).
Amongst my patients, the Non-Invasive Prenatal Test (NIPT) is now far more popular than the Nuchal Translucency Scan (NTS) and serum as a screening test for foetal chromosome disorders.
The cost has reduced considerably from what it was when NIPT screening was introduced and now through Sonic Genetics (Douglass Hanly Moir Pathology (DHM)), the NIPT testing is done in Australia. The cost of the Harmony NIPT through Sonic Genetics (DHM) has been reduced to $500.
The NTS looks at the skin fold on the back of the baby’s neck at about 12 weeks. This has been further refined by looking at the nose bone of the baby. In addition, there is a checking of the levels of two pregnancy hormones to increase accuracy. This is the combined test (ultrasound scan and serum) has a considered predictive value of about 92%. In contrast, the NIPT has >99.9% accuracy in checking for the three commonest chromosome disorders and as well can check for sex chromosome disorders and so the sex of your baby.
Sonic Genetics report a low-risk result as <1 in 10,000 risk of the checked chromosome having an abnormality. Checking for sex chromosome disorders and the sex of your baby is not possible with the NTS.
Women with a ‘high risk’ NTS result they are offered chorionic villous sampling (CVS) or amniocentesis. These are invasive tests that carry a miscarriage risk of about 1:200 to 1:300. How ‘high risk’ is usually defined is when the risk of miscarriage with a CVS or amniocentesis is less than the risk of the chromosome abnormality. Usually, now a woman with ‘high risk’ NTS will opt for an NIPT check.
What is Non-Invasive Prenatal Testing?
Chromosomal abnormalities (such as Down syndrome) are abnormalities of the baby’s DNA (which is the ‘blueprint” of the human body).
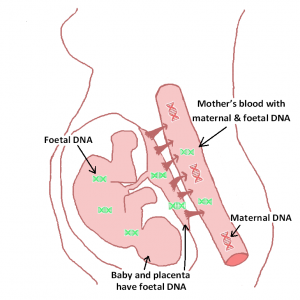
DNA originating from placental microparticles of the trophoblast of the placenta is shed into the mother’s bloodstream from as early as four weeks pregnant. This placental DNA is called cell free DNA (cfDNA) and is almost always the same as baby’s DNA. The amount of cfDNA increases as the pregnancy progresses. CfDNA diminishes quickly after the birth of the baby so that it is no longer detectable in the maternal blood approximately two hours after birth. CfDNA is significantly smaller in size than the maternal DNA in the bloodstream. NIPTing uses the smaller size of cfDNA to distinguish it and extract it from the maternal DNA.
A blood sample taken from the pregnant mother at any time in the pregnancy from approximately 10 weeks on usually has enough of her baby’s placental DNA that can be checked for the commonest chromosomal disorders. Sonic Genetics reports the percentage CfDNA in the specimen of maternal blood. The higher the percentage the more accurate the result.
The result of the simple blood test is predictive to more than 99.9% for Down Syndrome (Trisomy 21).
So the NIPT:
- is more accurate than NTS and serum in detecting the commonest chromosomal abnormalities (Trisomy 21, 13 and 18),
- has considerably fewer false-positive results than the NTS and serum. So the need for invasive testing by CVS or amniocentesis is reduced considerably.
- can check for sex chromosome disorders. This is not possible with an NTS and serum.
- can check the sex of your baby (if you want).
- Cane be done at 10 weeks pregnancy on, which is an earlier gestation than NTS screening (12 weeks)
Who does the NIPT screening?
With NTPT screening growing in popularity the cost has come down and there are now more options where you can go to get the testing done. Testing can now be done in Australia by Douglass Hanly Moir’s genetic testing facility called Sonic Genetics and by Genea IVF. Sonic Genetics uses Ariosa Diagnostics (USA laboratory) analysis kit locally under licence.
I was referring to another company until Sonic Genetics started doing the testing locally. My preference is now for blood collection to be done by Douglass Hanly Moir (DHM) and analysis to be done by Sonic Genetics. Analysis is done in Australia using the Harmony kit (under licence) which is owned by the American Lab Ariosa Diagnostics.
I have used DHM for pathology ever since I have been in private practice. I have always found DHM to be a high-quality laboratory that wants the greatest accuracy possible with reporting. They are also very efficient and are very easy to work with, discuss results with when needed, etc. DHM in the past was offering the NIPT service with overseas analysis and at a higher cost so I was using another company which uses another American laboratory kit locally under licence.
More NIPT information is shown in the table below.

Who has NIPT screening?
I offer the screening test option to all my patients.
A pregnant woman attending a public hospital as a public patient is unlikely to be offered NIPT screening at the antenatal clinic. I suspect this is because of financial considerations, as there is no Medicare rebate on the test.
In my experience, most GPs don’t at this stage know about the testing or know enough about the testing to offer it to their patients. So most GPs discuss only NTS screening. As well there being no Medicare rebate would be a deterrent for many GPs to offer the test.
So I still need a 12-week ultrasound scan?
An NIPT is much more accurate than an NTS in checking for chromosomal abnormalities. You don’t need both. An NTS, in addition, will not increase the accuracy of detection of Trisomy 21, 13 or 18.
The companies that do the NTS will encourage you to have an NTS type scan also. They will say it is to check for and detect developmental abnormalities sooner and to assess whether you are at higher risk of early-onset preeclampsia.
A 12-week ultrasound scan can check for some structural abnormalities in your baby such as exomphalos, holoprosencephaly, some heart abnormalities and megacystis. These may exist without a chromosomal abnormality. These abnormalities and more abnormalities will be checked for at your 19-week morphology scan. At the 19-week morphology scan, your baby will be bigger and so accuracy in detecting abnormalities will be greater. Also, other structural abnormalities will be checked for that are not apparent at 12 weeks. Neural tube defects (spina bifida) will be checked at the 19-week morphology scan.
A 12-week ultrasound scan will help predict your likelihood of developing preeclampsia in your pregnancy and if you are found to be at ‘high risk’ severe early-onset pre-eclampsia can be prevented by taking low-dose aspirin throughout your pregnancy. In the report ‘Early Administration of Low-Dose Aspirin for the Prevention of Severe and Mild Preeclampsia: A Systematic Review and Meta-Analysis’ Stéphanie Roberge, Yves Giguère, Pia Villa, Kypros Nicolaides, Merja Vainio, Jean-Claude Forest, Peter von Dadelzen, Daniel Vaiman, Sylvie Tapp, Emmanuel Bujold, Am J Perinatol 2012;29:551–556. it is stated low-dose aspirin started before 16 weeks pregnancy can prevent severe early onset preeclampsia. It also is concluded that “definitive trials are required to determine whether low-dose aspirin can prevent the adverse maternal and perinatal consequences of severe preeclampsia in high-risk women who may be identified through predictive screening programs”.
Severe early-onset preeclampsia is very uncommon and most preeclampsia is late onset. It is considered low-dose aspirin is not likely to prevent late-onset preeclampsia. An excellent article on early detection of preeclampsia is ‘Early Detection of Maternal Risk for Preeclampsia’ B. Mikat, A. Gellhaus, N. Wagner, C. Birdir, R. Kimmig, A. Köninger ISRN Obstet Gynecol. 2012;2012:172808. Epub 2012 Jul 17.’
While the exciting recent developments of looking at various biophysical and biochemical markers and maternal risk factors in determining the likelihood of developing preeclampsia is very promising, it is generally concluded further evaluation is needed. For the present, these new approaches are not endorsed as routine screening procedures by the Colleges that train and register obstetricians in Australia and New Zealand (RANZCOG), in the United Kingdom (RCOG) or in the USA (ACOG).
Preeclampsia is much more common in the first ongoing pregnancy than subsequent ongoing pregnancies with the same partner and so the value of biophysical and biochemical checking in subsequent pregnancies, when there are no maternal risk factors, is very questionable.
Checking for your maternal risk factors for preeclampsia is a normal part of your antenatal care. There are situations when low-dose aspirin is indicated.
I certainly have no objections to you having a 12-week ultrasound scan, but whether you have this done is your personal decision. It will cost you more money.
Are there problems the NIPT test will not detect?
Yes. The NIPT Test will only check for Trisomy 21 (Down syndrome), Trisomy 18 (Edwards’s Syndrome), Trisomy 13 (Palau’s Syndrome) and sex chromosomes disorders (Monosomy X, Klinefelter syndrome, etc.) Other chromosome disorders can’t be checked for. No chromosome disorders structural and developmental disorders) will not be checked for.
What are the limitations of the NIPT Test?
- NIPT testing does not screen for all foetal abnormalities. NIPT is very specific about the chromosomes it is screening for. Patients who themselves carry a chromosomal abnormality or who have had a transplant or stem cell therapy are not suitable for NIPT. IVF pregnancies with donor eggs and multiple pregnancies have specific restrictions with some NIPT tests.
- A negative NIPT does not completely rule out the chromosomal abnormalities that it is testing for.
- A positive NIPT does not mean the abnormal chromosomal result is certain but that there is a>50% chance. Diagnostic testing (CVS or amniocentesis) is recommended following a positive result.
- Medicare does not cover any of the cost of the NIPT.
- Occasionally there is no result with NIPT screening, despite a redraw of maternal blood for analysis.

