The reason for the question is the patient is anxious about this and is concerned the umbilical cord being around baby’s neck (nuchal cord) will adversely affect baby’s wellbeing. The worry is that the umbilical cord being around baby’s neck will result in reduced blood flow in the cord and that will cause reduced oxygenation of baby and so foetal distress or even foetal death.
There is nothing that can be done if the cord is around baby’s neck during the pregnancy except a Caesarean section delivery. To do an emergency Caesarean section at an earlier gestation or even at term gestation when there is no other reason is not considered warranted or appropriate management.
The umbilical cord being around baby’s neck is common and is found to be so at about 60 % of deliveries. While it is common for the umbilical cord to be around baby’s neck, a nuchal cord usually does not cause any problems during the pregnancy or in labour.
When there is foetal distress in labour and it is found at delivery that the umbilical cord is around baby’s neck the patient is told this and is advised that the nuchal cord may have been the reason for the foetal distress. But this is not known with certainty.
There can be other umbilical cord issues that can cause foetal distress. These include a knot in the umbilical cord, compression of the cord between baby’s head and the sidewall of the pelvis, baby entanglement in the cord and an unusually short umbilical cord.
Sometimes when tragically a patient has a stillborn baby it is apparent that it was due to a cord accident. At delivery there may be seen unusual twisting of the umbilical cord or a tight knot in the cord with the cord proximal to the cord segment swollen with blood and the cord part distal with pallor and no or minimal blood indicating that the cord accident cut off blood flow to baby. Sometimes the baby is entangled in the cord and so it is very possible that could have adversely affected blood flow in the cord and caused foetal demise.
On occasions, I do become concerned about there being increased risk of an umbilical cord problem in pregnancy that could adversely affect baby’s wellbeing. I was recently concerned about this with Mel’s unborn baby.
I recently managed Mel’s third pregnancy. She had an unstable lie of baby in the third trimester of her pregnancy. This had not been the case in the previous two pregnancies, which I also managed.
At antenatal visits from 29 weeks, I found her baby had repeatedly switched from cephalic (head down) to breech (bottom down). Her baby presentations at antenatal visits in the third trimester were cephalic, then breech, then breech, then cephalic, then breech and then at 37 weeks 6 days cephalic. Liquor volume was normal. At 37 weeks 6 days her baby was head down, but baby’s head was high and not engaged and her cervix was closed. I booked her for coming in that evening for prostaglandin ripening of the cervix and then induction of labour. Mel and I were both keen to avoid a Caesarean section after two previous uneventful vaginal deliveries. On the other had I was worried that with such excessive mobility of baby there could be a cord entanglement that could adversely affect baby’s wellbeing. I gave her an injection of Celestone Chronodose, a steroid to help mature baby’s lungs and reduce the risk of baby having breathing issues because she was 37 weeks 6 days gestation.
That night I had a call from the midwife. Mel had attended for induction cervical ripening. The midwife told me the baby’s head was no longer in the pelvis but was to the side. The baby had done another flip in the short time between when I saw her that day in my office and when she attended the Birth Unit. Prostaglandin ripening of the cervix was not done. I attended the next morning. An ultrasound scan by me showed the baby was now lying almost transverse. I could not turn the baby, so it was head down. As well her cervix was still closed and unfavourable for induction. Mel was given another injection of Celestone Chronodose and after CTG monitoring of baby was sent home. Mel was aware of my increasing concern that with such excessive mobility of baby there could be umbilical cord entanglement that could adversely affect baby’s wellbeing. On the other hand, Mel did not want a Caesarean section delivery. While Mel understood the umbilical cord risk, Mel is extremely sensible and is not prone to unnecessary anxiety. She is a delightful person and very easy to manage.
I next saw Mel in my office four days later. Baby was cephalic and Mel’s cervix was inducible. While her cervix was long, I could now pass my finger through the internal os of the cervix. Baby’s head was still high, but I could tip it with my finger through the internal os of the cervix. We were both excited that her labour could now be induced.
It was in the morning I saw her. I phoned the Birth Unit and persuaded the midwife to admit Mel that day for induction of labour. I advised she would need a Syntocinon infusion commenced first to initiate contractions that would push baby’s head down, so it was better applied to her cervix.
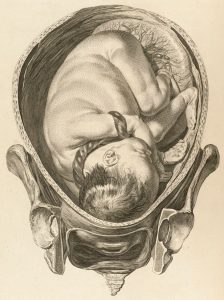
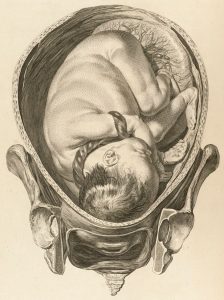
I then attended and did a stabilising induction of labour. While Mel was contacting baby’s head was still in the brim of the pelvis. The midwife pushed abdominally baby down towards the pelvis, so baby’s head was better applied to the cervix. I then did a slow careful rupture of membranes. The liquor was released slowly. I kept my finger in the cervix internal os and the midwife continued pressing baby down toward the pelvis until the liquor stopped flowing. The stabilising induction was done to help keep baby cephalic (head down) and minimise the risk of there being umbilical cord prolapse with a gush of liquor coming out. The stabilising induction worked. Baby head was now better applied to her cervix. Mel was kept upright in a sitting position on the bed until the labour was more established. There was careful monitoring of baby to make sure there was not suggestion of umbilical cord compression.
Mel’s labour progressed uneventfully. She went on to have spontaneous vaginal delivery. Her perineum was intact. Baby’s umbilical cord was four times around baby’s neck. Despite the cord being four times around baby’s neck there was no hint of foetal distress in labour and baby was born in excellent condition. Baby’s birth weight was 3198gms. Mel was keen to go home and be with her other children. In accord with her wish, she was discharged four hours after delivery. I will be next seeing her for her six-week postnatal visit.
The umbilical cord being four times around baby’s neck was most likely a consequence of baby having an unstable lie. While I was concerned about baby having a cord accident, nothing else could have been done except a Caesarean section, which was not Mel’s wish. Mel understood the cord accident risk but wanted a vaginal delivery if possible. I supported her in this decision. With very careful management, Mel achieved her goal. Despite the cord being four times around baby’s neck there was no foetal distress and baby was born in excellent condition.