Caesarean section is either an emergency or elective operation.

An emergency Caesarean section is done when there is an urgent complication in pregnancy or labour which significantly compromises your or your baby’s wellbeing (or both). This implies that continuing the pregnancy or labour for a significant time will be very dangerous. How quickly the Caesarean needs to be done will vary from extremely urgent (viz. immediately) to within the next few hours. An elective Caesarean section is a pregnancy planned event. The reason could be previous pregnancy or labour problems, maternal health issues, complications in this pregnancy and sometimes a patient’s personal request (without any obstetric indications). Some women prefer to have a Caesarean section rather than a vaginal birth. I am agreeable to this personal choice as long as the risks are understood. An elective Caesarean section is booked on a date close to term (usually 38 to 39 weeks pregnancy). It is safer to avoid the onset of labour. If you are booked for an elective Caesarean section and you go into labour before the scheduled date please advise the hospital and attend immediately. I will do your Caesarean section as soon as possible after you arrive at the hospital, irrespective of the hour of the day.
a
a
Theatre Procedures
Before you arrive in the operating theatre.
- You will be prepared for theatre in your room on the postnatal ward for an elective Caesarean section. For an emergency Caesarean section you will be prepared for theatre in the Birthing Unit (San Hospital) and in the Birth Unit (Norwest Private Hospital).
- You should be fasting for six hours at least before a Caesarean section. Sometimes this is not possible with an emergency Caesarean section.
- You will be given a top pubic shave (if needed)
- You will be given Sodium Citrate drink (to neutralise acids in your stomach in case a general anaesthetic is needed).
- You will also need to sign a hospital consent form for a Caesarean section. If elective this will have been done in my office. Please remember to bring your completed consent form to the hospital with you.
- You will be taken to an area in the theatre complex but outside the actual operating theatre on a trolley (with your midwife escorting at Norwest Private and emergency at the San Hospital).
- When you arrive at the theatre complex your personal details will be checked and you will have a consultation with the anaesthetist (if this has not already happened).
In the operating theatre or in anaesthetic bay adjacent to the operating theatre.
- An intravenous line will be set up by the anaesthetist if you don’t have one already
- The anaesthetist will then administer the regional anaesthetic which is usually spinal or spinal with epidural anaesthetic. A spinal anaesthetic is considered safer than a general anaesthetic. Also, you can see your baby immediately after birth and your husband can stay with you in theatre.
- If it is an emergency Caesarean section and you have been in labour with an epidural in place as this will usually be used instead.
In the operating theatre
- Once the anaesthetic is working I or my surgical assistant will catheterise your bladder. This will usually be done usually before you ‘go to sleep’ if you have a general anaesthetic.
- I will then clean your abdomen with an antiseptic solution.
- I will place sterile drapes over your abdomen.
- If you are awake, and your husband/partner is with you, then he will be given a seat beside your head so he can support you and share in the joy with you.
- I will do the operation.
- I will have a surgical assistant to assist me with the operation.
- I will make a transverse cut in your skin about 10 cm long (width of your baby’s head) and about 1 cm below the pubic hairline. If you have a scar I will use the same incision line with excision of the old scar.
- The drape runs vertically from your chest so you can’t see the operation happening.
- When I am delivering your baby I will ask the staff to lower the drapes so you and your husband/partner can see your baby being born.
- I will encourage your husband/partner to take lots of photos. Sometimes the anaesthetic sister will offer to do this for you.
- I will invite you to touch your baby’s foot.
- There can be delayed cord clamping if you request and as long as there is no concern about baby’s wellbeing or you wish cord blood collection.
- Your baby will be given to the midwife attending and taken to the baby table for checking and wrapping on the newborn resuscitaire unit.
- Your husband/partner can cut the umbilical cord at this time.
- Your baby will then be brought back to you and will stay with you and your husband/partner as long as possible. If ‘baby or family friendly’ this should be through the rest of the operation. If not ‘baby or family friendly’ is is as long as it is possible for the midwife you remain in theatre. Sometimes there is concern about baby’s wellbeing and if so baby will need to be taken to the Special Care Bay Unit (SCBU).
- There can be some ‘skin-to-skin’ contact but this is less than with a vaginal delivery because of theatre sterile drapes. Full ‘skin-to-skin’ contact and breast feeding will be offered in recovery ward.
- My closure technique Baby-friendly in detail in the blog titled ‘Caesarean section closure techniques‘.
- Skin wound closure is with a special subcuticular stitch that dissolves.
- At the end of the operation, a special dressing over your wound and the drapes are removed
- A rectal suppository for pain relief will sometimes be administered at the end of the operation. Some anaesthetists use intravenous analgesics instead.
- You will be taken from the operating theatre to the recovery ward and then to the postnatal ward. If it is a ‘baby friendly’ (San) / ‘family friendly’ (Norwest) Caesarean section then your baby and your husband/partner will stay with you in the recovery ward.
- In recovery ward you (and your husband/partner if baby or family friendly) will have opportunity to cuddle your baby, you will be able to have ‘skin-to-skin’ contact with baby, and you can start breast feeding your baby.
Husband/partner in theatre
- Your husband/partner is encouraged to be with you for support in operating theatre. This is another reason for a regional anaesthetic. Make sure he brings the camera so he can take lots of baby photos of your baby being born and afterwards.
- Your husband/partner will be invited by eth midwife to cut the umbilical cord once baby is on on the newborn resuscitaire unit.
- If it is general anaesthetic then the hospital usually rules your husband cannot be in the operating theatre. That is because he is there when you are awake to support you. But that is not the case if you are fully anaesthetised.
After your Caesarean section.
- If you have a ‘baby friendly’ (San) / ‘family friendly’ (Norwest) and there is not concern about baby’s wellbeing then your baby, your husband/partner and the midwife will stay with you in the recovery ward.
- If you are NOT having a ‘baby friendly’ (San) / ‘family friendly’ (Norwest) then your baby, your husband/partner and the midwife will go from the operating theatre to the postnatal ward while I am finishing the operation.
- You will go to recovery ward for the minimum time possible and then to your postnatal room to join your baby and husband.
‘Baby-friendly’ (San) / ‘family friendly’ (Norwest) Caesarean section
- ‘Baby-friendly’ (San) / ‘family friendly’ (Norwest) Caesarean section means your baby, your husband/partner and the midwife all stay with you in recovery ward and so you are not separated from your baby after birth.
- ‘Baby-friendly’ (San) / ‘family friendly’ (Norwest) are available at both hospitals. At the San, it is possible for both elective and emergency Caesarean sections to be ‘baby friendly’. At Norwest it is only possible for elective (NOT emergency) Caesarean sections to be ‘family friendly’ and only if the operation is started before 4.00pm, only if there are no more than five ‘family friendly’ in any one day and only if the Birth Unit is not too busy at the time of your delivery.
- If your baby is unwell after delivery or you have insulin-dependent diabetes then your baby will need to be admitted to SCBU and so it is not safe for you to have a ‘baby friendly’ (San) / ‘family friendly’ (Norwest) Caesarean section.
- I will request that you have a ‘baby friendly’ (San) / ‘family friendly’ (Norwest) Caesarean section if it is an elective procedure when we book your operation.
The next days
- The catheter and intravenous line are usually removed the day after.
- You will resume a normal diet.
- You are encouraged to be as ambulatory as you can as soon as possible the day after your Caesarean section.
- You will switch to oral analgesics, and you will be given a supply to take home if needed.
- As skin wound closure was with a special subcuticular stitch that dissolves, there is no stitch or staples to be removed.
- The special wound dressing I applied in theatre will remain on at discharge for the hospital. I encourage you to leave it on as long as possible as the longer it is left on the better looking the scar.
- If the dressing is still there I take it off at the six-week postnatal check-up.
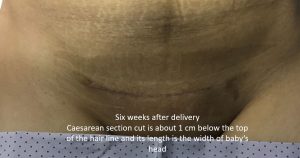
- Adjacent is a scar photographed at the six-week postnatal check-up just after I removed the dressing. This was the scar after this patient’s second Caesarean section.
- You can be discharged home when you and your baby are ready. Particularly patients who have had previous babies are often keen you be discharged early. Sometimes discharge is on the third postoperative day.
When you get home
- Rest for the first week then gradually resume normal activities.
- If you get tired or doing something hurts you then slow down.
- You can resume driving a car when pain-free. If you can do an emergency brake and it doesn’t hurt you then you can drive. I have had patients report they started driving two weeks after their Caesarean section.
- You can resume sexual relations when the lochia ceases but you will need contraception cover in case there is early ovulation.
- You can’t go swimming while you have lochia. the lochia implies the uterus has not fully healed.
- See me for your postnatal visit six weeks after your delivery.
See also:
- Caesarean section Delivery in our Question and Answers section
- Caesarean section closure technique in our Blog
